Best Treatment in Sciatica Pain
Introduction
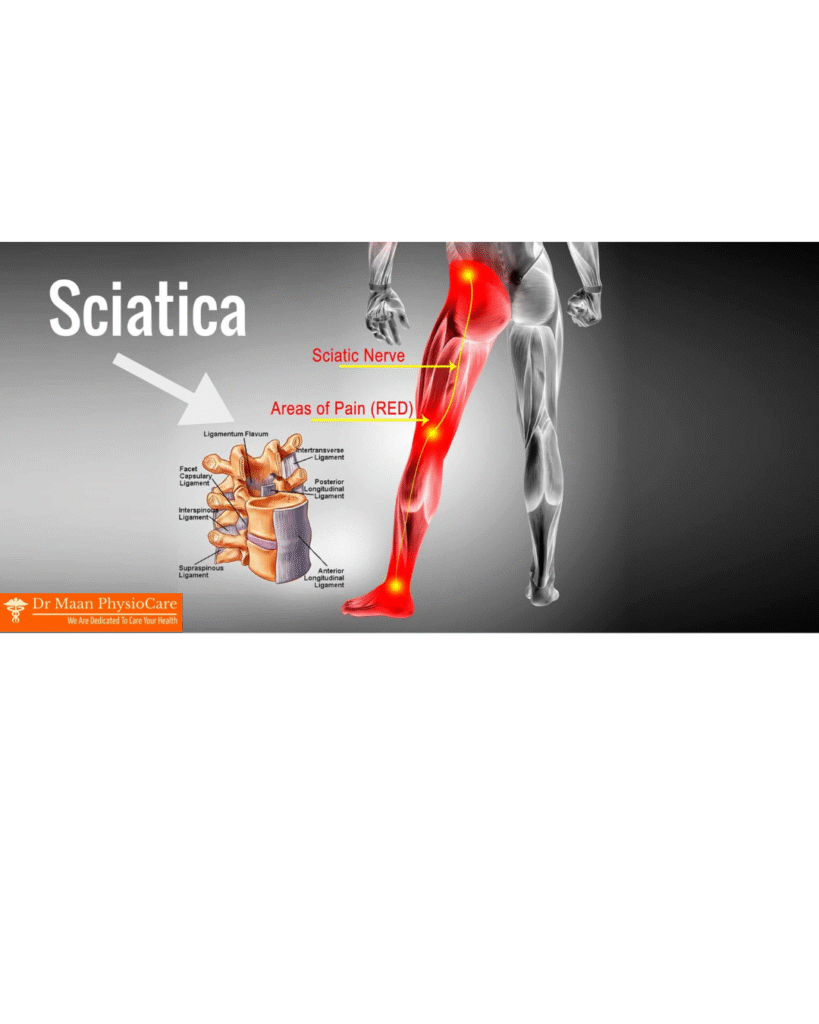
Sciatica is one of the most common and painful conditions affecting the lower back and legs. It refers to pain that radiates along the path of the sciatic nerve, which is the longest and thickest nerve in the human body. The sciatic nerve originates from the lower spine, passes through the buttocks, and travels down each leg to the feet. When this nerve becomes compressed, irritated, or inflamed, it causes pain that can range from mild to severe, often affecting daily activities and quality of life.
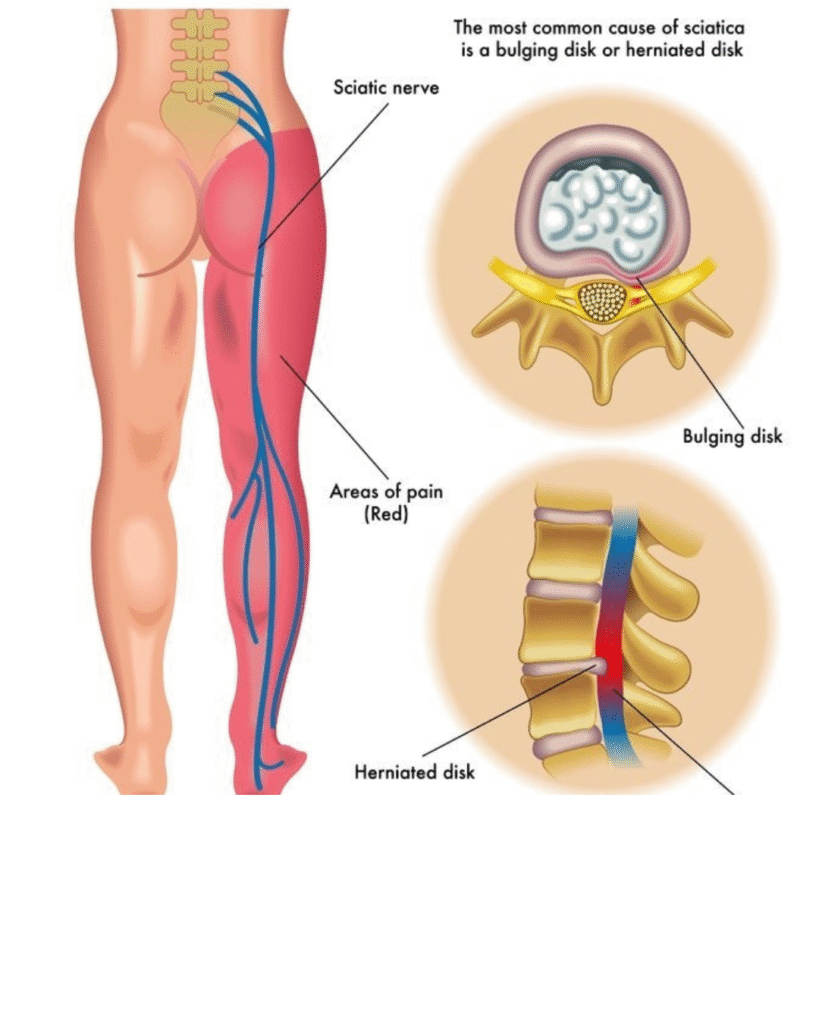
Sciatica is not a disease by itself but rather a symptom of an underlying medical condition such as a herniated disc, spinal stenosis, or degenerative disc disease. Understanding sciatica requires knowledge of spinal anatomy, nerve function, and the mechanical and inflammatory processes that lead to nerve irritation.
Anatomy of the Sciatic Nerve
The sciatic nerve originates from the lumbar and sacral spinal nerves (L4 to S3). These nerves join together in the lower spine to form a thick bundle that passes through the greater sciatic notch of the pelvis, runs beneath the piriformis muscle, and continues down the back of the thigh. In the thigh, the nerve splits into two main branches:
- The tibial nerve (which runs down the back of the leg), and
- The common peroneal or fibular nerve (which runs along the outer side of the leg).
The sciatic nerve controls sensation and muscle movement in the thighs, legs, and feet. Therefore, any irritation or compression along its pathway can cause pain, tingling, numbness, or weakness anywhere from the lower back to the toes.
Causes of Sciatica
Sciatica occurs when the sciatic nerve is compressed or irritated. The most common causes include:
1. Herniated or Slipped Disc
A herniated disc is the most frequent cause of sciatica. The spinal discs act as cushions between the vertebrae. When one of these discs bulges or ruptures, the inner gel-like substance can press on the nearby spinal nerves, including those that form the sciatic nerve. This pressure causes inflammation and pain that radiates down the leg.
2. Degenerative Disc Disease
With age, the spinal discs lose their flexibility and height, reducing the space between vertebrae. This can lead to nerve root compression or formation of bone spurs, both of which can pinch the sciatic nerve.
3. Spinal Stenosis
Spinal stenosis is the narrowing of the spinal canal. It can be due to aging, arthritis, or abnormal bone growths. When the canal narrows, it puts pressure on the spinal cord and the nerve roots, including those that form the sciatic nerve.
4. Spondylolisthesis
This condition occurs when one vertebra slips forward over the one below it. The slipped vertebra can compress the nerve roots and cause sciatica symptoms.
5. Piriformis Syndrome
The piriformis muscle, located deep in the buttock, can sometimes become tight or spasm. When this happens, it can irritate the sciatic nerve that passes directly beneath (or occasionally through) it, leading to pain that mimics sciatica. This is known as piriformis syndrome.
6. Trauma or Injury
Any direct injury to the lower back, pelvis, or thigh can damage or irritate the sciatic nerve.
7. Tumors or Infections
In rare cases, tumors growing in or near the spine can compress the sciatic nerve. Similarly, infections such as abscesses can cause inflammation and nerve irritation.
8. Pregnancy
During pregnancy, hormonal changes and the additional weight of the baby can increase pressure on the spine and sciatic nerve, resulting in temporary sciatica.
Symptoms of Sciatica
The hallmark symptom of sciatica is pain that radiates from the lower back down to the leg. The intensity and nature of pain vary among individuals, depending on the severity of nerve compression.
Common Symptoms:
- Pain:
- Often starts in the lower back or buttock and radiates down the leg.
- The pain may be sharp, burning, or electric shock-like.
- It usually affects one side of the body.
- It may worsen with coughing, sneezing, or prolonged sitting.
- Numbness and Tingling:
- A “pins and needles” sensation may occur in the leg or foot.
- Weakness:
- Muscle weakness in the affected leg can occur, making it difficult to move or lift the foot (foot drop).
- Limited Mobility:
- Patients may have difficulty walking, standing, or bending due to pain.
- Postural Changes:
- Many people lean to one side or adopt a bent posture to relieve pressure on the nerve.
Pain Pattern:
- If L4 is affected → pain may radiate to the thigh and knee.
- If L5 is affected → pain may go to the outer leg, top of the foot, and big toe.
- If S1 is affected → pain may go to the outer foot, heel, or little toe.
Diagnosis of Sciatica
Diagnosing sciatica begins with a detailed medical history and physical examination. The doctor will ask about the onset of pain, its location, intensity, and any aggravating or relieving factors.
1. Physical Examination
- Straight Leg Raise (SLR) Test: The patient lies on their back, and the doctor raises one leg. Pain that shoots down the leg when the leg is raised between 30°–70° suggests sciatic nerve irritation.
- Neurological Examination: Tests muscle strength, reflexes, and sensation in the legs.
2. Imaging Tests
- X-rays: Show bone alignment, fractures, or bone spurs.
- MRI (Magnetic Resonance Imaging): The most accurate test to visualize discs, nerves, and soft tissues.
- CT Scan: Useful when MRI is not available or contraindicated.
- Electromyography (EMG): Measures the electrical activity of muscles to assess nerve damage.
Treatment of Sciatica
The treatment of sciatica depends on the underlying cause, severity of symptoms, and duration of pain. Most cases improve with conservative (non-surgical) treatments within a few weeks. Surgery is considered only when symptoms persist or worsen.
1. Conservative (Non-Surgical) Treatment
a. Rest and Activity Modification
Short periods of rest may help, but prolonged bed rest is not advised. Light activities such as walking and stretching promote recovery and reduce stiffness.
b. Medications
- Pain relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen reduce pain and inflammation.
- Muscle relaxants: Help relieve muscle spasms.
- Neuropathic pain medications: Drugs such as gabapentin or pregabalin can help with nerve-related pain.
- Corticosteroids: Oral or injected steroids may reduce inflammation around the nerve root.
c. Physiotherapy
Physiotherapy is the cornerstone of sciatica management. It focuses on reducing pain, restoring mobility, and strengthening the back and core muscles.
Key techniques include:
- Stretching exercises: Especially hamstring and piriformis stretches.
- McKenzie exercises: Help reduce disc-related nerve pressure.
- Core strengthening: Strengthens abdominal and lower back muscles.
- Postural training: Teaches proper body mechanics to prevent recurrence.
- Modalities: Ultrasound, TENS (Transcutaneous Electrical Nerve Stimulation), and heat therapy for pain relief.
d. Hot and Cold Therapy
Cold packs reduce inflammation in the initial stages, while heat therapy improves blood circulation and relaxes tight muscles.
e. Epidural Steroid Injections
When oral medications are insufficient, corticosteroids can be injected near the affected nerve root to reduce inflammation and pain.
2. Surgical Treatment
Surgery is reserved for severe cases, especially when:
- There is loss of bowel or bladder control (cauda equina syndrome).
- There is progressive leg weakness or paralysis.
- Pain persists for more than 3 months despite conservative treatment.
Common Surgical Options:
- Discectomy/Microdiscectomy: Removes part of the herniated disc pressing on the nerve.
- Laminectomy: Removes part of the vertebral bone (lamina) to relieve spinal canal pressure.
- Spinal Fusion: Fuses two or more vertebrae to stabilize the spine.
Rehabilitation and Lifestyle Management
Recovery from sciatica requires long-term attention to posture, ergonomics, and fitness. Preventing recurrence is as important as treating the initial episode.
1. Exercise and Fitness
- Engage in regular physical activity such as swimming, yoga, or brisk walking.
- Strengthen core and back muscles through guided exercises.
- Maintain flexibility of hamstrings and hip muscles.
2. Ergonomics
- Use chairs with proper lumbar support.
- Adjust computer screens and desks to avoid slouching.
- Avoid lifting heavy weights improperly; always bend at the knees, not the waist.
3. Weight Management
Excess body weight increases stress on the spine. A balanced diet and regular exercise help reduce the risk of recurrence.
4. Proper Sleep Posture
Sleeping on the side with a pillow between the knees or on the back with a pillow under the knees helps reduce strain on the lower back.
Complications of Untreated Sciatica
If left untreated, severe or chronic sciatica can lead to:
- Permanent nerve damage
- Loss of sensation or strength in the affected leg
- Chronic pain syndrome
- Bowel or bladder dysfunction (in rare cases, cauda equina syndrome)
Therefore, timely medical evaluation and proper treatment are essential.
Prognosis (Outcome)
The majority of people with sciatica recover completely with conservative treatment within 6 to 8 weeks. However, recurrence is possible if lifestyle changes are not maintained. Regular physiotherapy, exercise, and ergonomic awareness significantly improve long-term outcomes.
Physiotherapist’s Role in Sciatica Management
A physiotherapist plays a crucial role in both pain relief and functional recovery. Their responsibilities include:
- Assessing the posture, gait, and muscle imbalances.
- Designing a personalized exercise program.
- Educating the patient about spine health.
- Applying electrotherapy modalities for pain control.
- Monitoring progress and preventing recurrence.
Physiotherapy not only treats the symptoms but also addresses the root mechanical cause of nerve compression.


Leave a Reply