Best Treatment In Parkinson’s Disease
Introduction
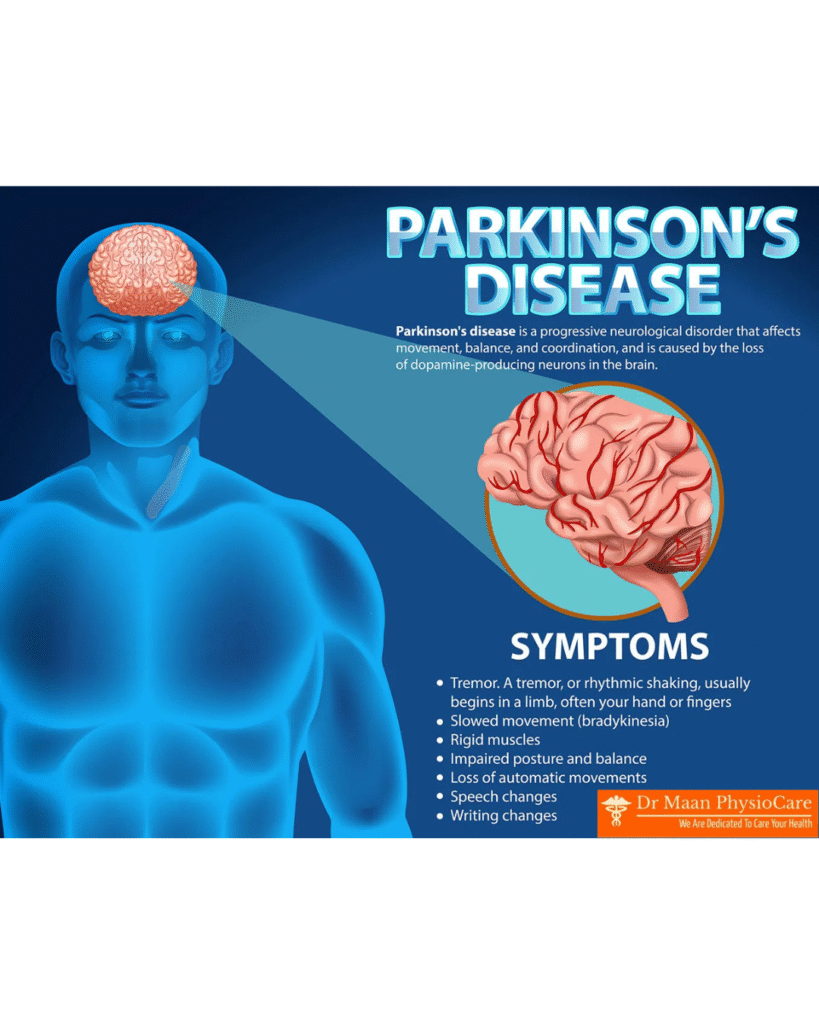
Parkinson’s Disease (PD) is a chronic, progressive neurological disorder that affects movement, muscle control, and coordination. It primarily occurs due to the degeneration of specific brain cells that produce dopamine—a neurotransmitter responsible for smooth and coordinated muscle activity. As dopamine levels drop, symptoms such as tremors, slowness of movement, stiffness, and balance problems gradually appear. Parkinson’s is most common in older adults, but it can also develop in younger individuals (known as Young-Onset Parkinson’s).
This condition progresses slowly and varies from person to person. While there is no permanent cure today, early diagnosis, medical treatment, physiotherapy, lifestyle modification, and regular follow-ups can significantly improve quality of life.
What Is Parkinson’s Disease?
Parkinson’s Disease is classified as a neurodegenerative disorder, meaning it involves the gradual damage and loss of nerve cells (neurons). The key affected area is the substantia nigra, a part of the midbrain responsible for producing dopamine. When these dopaminergic neurons die or deteriorate, the brain cannot send proper signals for movement.
By the time motor symptoms become noticeable, 60–80% of dopamine-producing cells are already damaged. This is why early detection is difficult.
PD is also known as a movement disorder but includes many non-motor symptoms as well.
Causes of Parkinson’s Disease
The exact cause is still unknown, but several factors contribute:
1. Genetic Factors
Some cases are caused by mutations in specific genes (LRRK2, PARK7, PINK1, etc.). However, genetically inherited Parkinson’s is rare and accounts for only 10–15% of cases.
2. Environmental Factors
Exposure to certain toxins increases Parkinson’s risk:
- Pesticides
- Herbicides
- Heavy metals
- Well-water contamination
Long-term exposure to these chemicals damages dopamine cells.
3. Age
Age is the biggest risk factor. Parkinson’s usually affects people above 60 years.
4. Oxidative Stress
Free radicals damage neurons over time, reducing dopamine production.
5. Mitochondrial Dysfunction
When the energy-producing parts of a cell malfunction, neurons become weak and die prematurely.
6. Repeated Head Injury
Frequent trauma to the brain (boxing, accidents) increases risk.
Pathophysiology – What Happens Inside the Brain?
The main changes in Parkinson’s Disease:
1. Loss of Dopamine
Dopamine is essential for:
- Smooth movements
- Postural control
- Coordination
- Motivation and cognitive function
Loss of dopamine leads to classic motor symptoms.
2. Lewy Body Formation
Inside the neurons, abnormal protein clumps called Lewy bodies accumulate. These interfere with normal cell function and eventually cause cell death.
3. Basal Ganglia Dysfunction
Parkinson’s affects the basal ganglia, the brain’s movement control center. Because of dopamine deficiency, the basal ganglia become overactive in some areas and underactive in others, leading to:
- Slowed movements
- Muscle rigidity
- Tremors
Signs and Symptoms
Parkinson’s Disease symptoms are divided into motor and non-motor symptoms.
A. Motor Symptoms
1. Tremors
The most common early symptom.
- Usually starts in one hand (“pill-rolling tremor”).
- Occurs at rest.
- Reduces during movement.
- Worsens with stress or fatigue.
2. Bradykinesia (Slowness of Movement)
Individuals experience:
- Difficulty initiating movement
- Slower walking
- Small steps (shuffling gait)
- Reduced blinking
- Difficulty writing (micrographia)
Bradykinesia is the hallmark symptom of PD.
3. Muscle Rigidity
Muscles become stiff, leading to:
- Pain
- Limited range of motion
- “Cogwheel” rigidity (jerky resistance during movement)
4. Postural Instability
Balance problems occur due to weak reflexes and poor posture.
This increases fall risk.
5. Gait Disturbance
Specific walking problems include:
- Shuffling
- Stooped posture
- Reduced arm swing
- Freezing of gait (sudden inability to move)
B. Non-Motor Symptoms
Non-motor symptoms are sometimes more disabling than motor symptoms.
1. Cognitive Symptoms
- Memory issues
- Slower thinking
- Problems with planning
- Dementia in later stages
2. Mood Disorders
- Depression
- Anxiety
- Apathy
- Irritability
These symptoms often appear early, even before motor symptoms.
3. Sleep Problems
- Insomnia
- REM sleep behavior disorder (acting out dreams)
- Restless legs syndrome
- Excessive daytime sleepiness
4. Autonomic Symptoms
The autonomic nervous system also gets affected:
- Low blood pressure
- Constipation
- Bladder problems
- Sweating
- Sexual dysfunction
5. Sensory Symptoms
- Loss of smell (hyposmia)
- Pain
- Tingling sensation
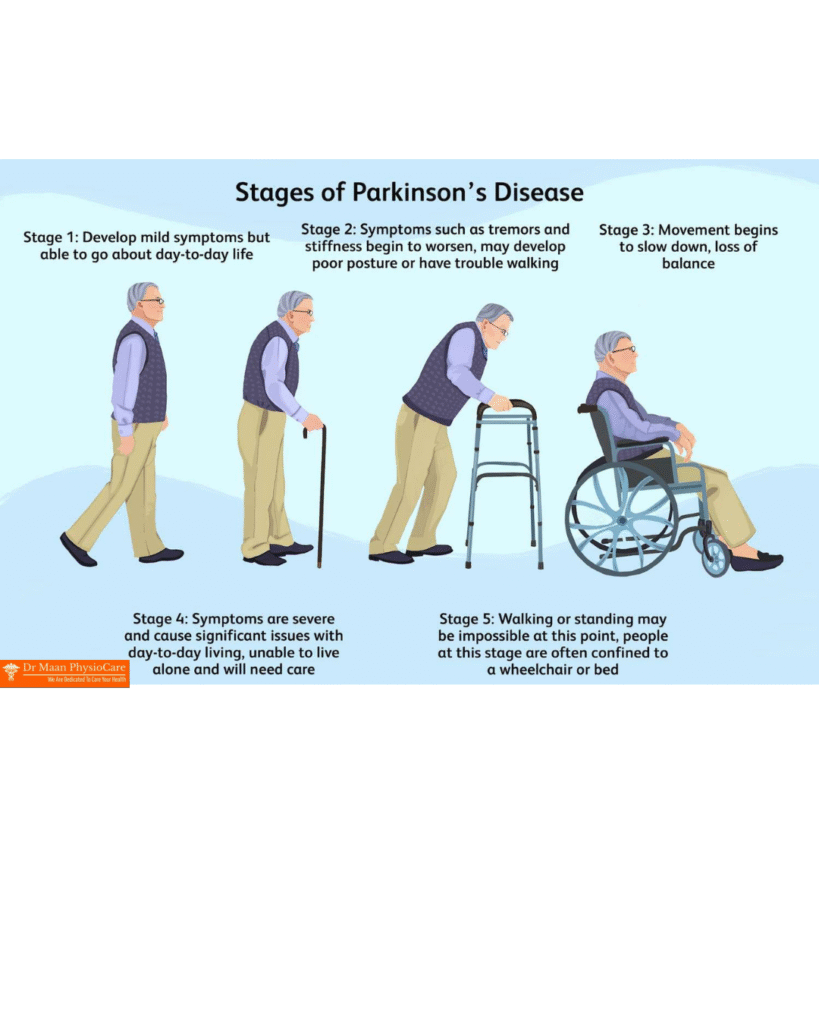
Stages of Parkinson’s Disease
Doctors often use the Hoehn and Yahr scale to classify progression:
Stage 1: Mild
- Symptoms on one side only
- Tremors or mild stiffness
- Daily activities normal
Stage 2: Moderate
- Symptoms on both sides
- Early walking problems
- Slower movements
Stage 3: Mid-stage
- Falls begin
- Significant bradykinesia
- Patient still independent
Stage 4: Advanced
- Severe stiffness
- Limited mobility
- Help required for daily tasks
Stage 5: Severe
- Wheelchair or bed-bound
- Severe cognitive impairment possible
Diagnosis of Parkinson’s Disease
There is no single test. Diagnosis is clinical, based on:
- Medical history
- Neurological examination
- Symptom pattern
- Response to dopamine medications
In some cases:
- MRI
- PET scan (DaTscan)
- Blood tests
are used to rule out other conditions.
Early diagnosis is challenging because symptoms are subtle.
Treatment of Parkinson’s Disease
There is no cure, but many treatments help control symptoms and improve quality of life.
1. Medications
a. Levodopa
The most effective medication.
It converts into dopamine inside the brain and reduces bradykinesia, rigidity, and tremor.
b. Carbidopa
Given with Levodopa to reduce side effects and increase absorption.
c. Dopamine Agonists
(Ropinirole, Pramipexole)
Mimic the action of dopamine.
d. MAO-B Inhibitors
(Rasagiline, Selegiline)
Prevent dopamine breakdown.
e. COMT Inhibitors
Prolong the effect of Levodopa.
f. Anticholinergics
Help in reducing tremors.
Medication effectiveness varies from person to person.
2. Surgical Treatment – Deep Brain Stimulation (DBS)
DBS is recommended for advanced Parkinson’s with severe tremors or medication fluctuations.
Procedure:
- Electrodes are implanted into specific brain regions
- A pulse generator is placed in the chest
- Electrical signals regulate abnormal brain activity
It improves motor symptoms but does not stop disease progression.
3. Physiotherapy
Rehabilitation plays a crucial role in maintaining mobility and independence.
Goals of physiotherapy:
- Improve gait
- Maintain posture
- Enhance balance
- Reduce rigidity
- Increase flexibility
- Prevent falls
Therapeutic approaches:
- Strength training
- Stretching exercises
- Gait training
- Balance exercises
- Cueing techniques (visual/auditory cues)
- Task-specific exercises
- Breathing exercises
Physiotherapy significantly improves quality of life.
4. Occupational Therapy
Helps with daily activities such as:
- Dressing
- Eating
- Writing
- Using the toilet
- Safety at home
Assistive devices may also be recommended.
5. Speech Therapy
Many patients experience voice weakness and swallowing difficulty.
Speech therapists help with:
- Voice training
- Articulation
- Breath control
- Swallowing exercises
6. Lifestyle Management
Exercise
Daily exercise improves:
- Mobility
- Balance
- Mood
- Overall disease progression
Recommended activities:
- Walking
- Cycling
- Yoga
- Tai chi
- Swimming
- Dancing
Diet
No specific “Parkinson’s diet,” but:
- High-fiber foods
- Hydration
- Antioxidant-rich fruits
- Omega-3 fatty acids
help reduce symptoms such as constipation and inflammation.
Mental Health Care
Counseling, meditation, and social engagement help manage depression and anxiety.
Complications of Parkinson’s Disease
If not managed properly, complications may include:
- Falls and fractures
- Severe swallowing difficulty
- Pneumonia
- Cognitive decline
- Inability to perform daily activities
- Depression
Early treatment and rehabilitation significantly reduce complications

Leave a Reply