Piriformis Syndrome Treatment Without Surgery
Piriformis Syndrome is a common but often misdiagnosed cause of buttock pain and leg pain. Many people mistake it for sciatica or a spine-related problem, but in reality, the pain originates from a small muscle deep in the hip region called the piriformis muscle. With the rise of sedentary lifestyles, long sitting hours, and poor posture, Piriformis Syndrome is becoming increasingly common among office workers, drivers, athletes, and elderly individuals.
This blog explains what Piriformis Syndrome is, why it occurs, how to identify it, and how physiotherapy plays a vital role in its treatment and recovery.
What Is Piriformis Syndrome?
The piriformis muscle is a small, flat, pear-shaped muscle located deep in the buttock region. It originates from the front of the sacrum (lower spine) and attaches to the upper part of the femur (thigh bone). Its primary functions include:
- External rotation of the hip
- Stabilizing the hip joint
- Assisting in walking and balance
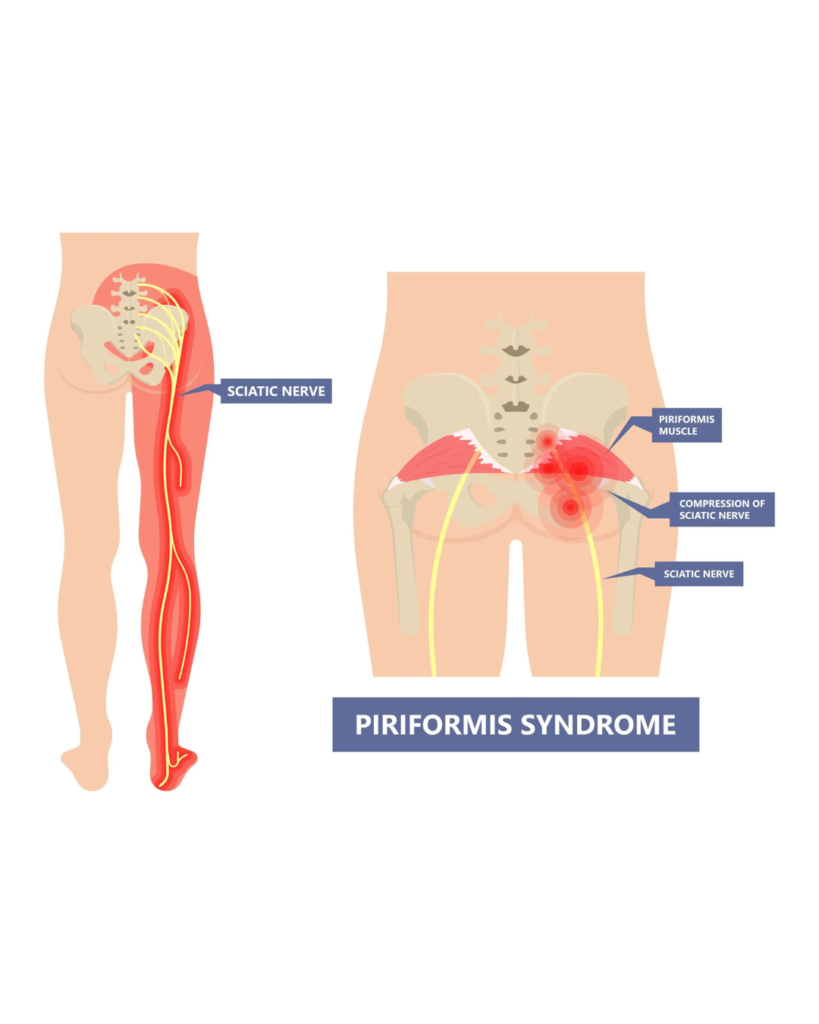
The sciatic nerve, the longest and thickest nerve in the human body, passes very close to the piriformis muscle. In some individuals, the nerve passes directly beneath the muscle, while in others, it may pass through or over it. When the piriformis muscle becomes tight, inflamed, or goes into spasm, it can compress the sciatic nerve, leading to pain and neurological symptoms. This condition is known as Piriformis Syndrome.
Causes of Piriformis Syndrome
Piriformis Syndrome can develop due to several reasons, often related to lifestyle, posture, or muscle imbalance. Common causes include:
- Prolonged Sitting
Long hours of sitting, especially on hard surfaces, increase pressure on the piriformis muscle. - Poor Posture
Slouching, uneven sitting, or improper spinal alignment can strain the hip muscles. - Muscle Overuse or Strain
Sudden increase in physical activity, running, cycling, or heavy exercise without warm-up. - Trauma or Injury
A fall on the buttock or hip area can cause inflammation of the piriformis muscle. - Muscle Imbalance
Weak gluteal muscles and tight hip rotators increase stress on the piriformis. - Anatomical Variations
In some individuals, the sciatic nerve passes through the piriformis muscle, increasing the risk of compression.
Symptoms of Piriformis Syndrome
Symptoms can vary from mild discomfort to severe pain and may worsen over time if left untreated.
Common Symptoms Include:
- Deep pain in the buttock region (usually on one side)
- Pain that worsens while sitting, driving, or climbing stairs
- Radiating pain from buttock to thigh or leg
- Tingling, numbness, or burning sensation in the leg
- Pain during hip movement or prolonged walking
- Difficulty sitting for long periods
Unlike spinal sciatica, lower back pain may be minimal or absent in Piriformis Syndrome.

Physiotherapy plays a key role in the effective, non-surgical treatment of Piriformis Syndrome. Since this condition mainly occurs due to muscle tightness, spasm, weakness, and postural imbalance, physiotherapy focuses on correcting these underlying causes rather than just controlling pain. With early and proper physiotherapy intervention, most patients achieve complete recovery and return to normal daily activities without the need for surgery or long-term medication.
Goals of Physiotherapy in Piriformis Syndrome
The primary objectives of physiotherapy treatment are:
- To reduce pain and inflammation
- To relieve pressure on the sciatic nerve
- To relax the tight piriformis muscle
- To improve hip mobility and flexibility
- To strengthen weak muscles around the hip and pelvis
- To correct posture and movement patterns
- To prevent recurrence of symptoms
Assessment Before Physiotherapy Treatment
Before starting treatment, a physiotherapist performs a thorough assessment, which includes:
- Detailed history of pain (onset, duration, aggravating factors)
- Postural assessment
- Gait analysis
- Palpation of piriformis and surrounding muscles
- Range of motion testing of hip and lumbar spine
- Special tests (FAIR test, Pace sign)
- Rule out spinal causes such as disc prolapse
This assessment helps in creating a personalized treatment plan.
Pain Relief Modalities in Physiotherapy
In the acute phase, pain control is the first priority.
Electrotherapy Modalities
- Interferential Therapy (IFT): Reduces deep muscle pain and spasm
- Transcutaneous Electrical Nerve Stimulation (TENS): Controls nerve-related pain
- Ultrasound Therapy: Reduces inflammation and improves tissue healing
Thermotherapy
- Hot pack: Relaxes tight muscles and improves blood circulation
- Cold pack: Used in acute inflammation to reduce pain and swelling
These modalities help prepare the muscle for further manual therapy and exercises.
Manual Therapy Techniques
Manual therapy is highly effective in Piriformis Syndrome.
Soft Tissue Mobilization
- Deep tissue massage
- Myofascial release
- Trigger point therapy
These techniques reduce muscle tightness and relieve pressure on the sciatic nerve.
Joint Mobilization
- Hip joint mobilization
- Sacroiliac joint mobilization (if required)
Manual therapy improves joint movement and reduces compensatory stress.
Stretching Exercises for Piriformis Syndrome
Stretching is a core component of physiotherapy management.
Key Stretching Exercises
- Supine piriformis stretch
- Sitting piriformis stretch
- Figure-of-four stretch
- Hip external rotator stretch
- Hamstring and iliotibial band stretch
Stretching should be:
- Performed slowly
- Pain-free
- Held for 20–30 seconds
- Repeated 3–5 times


Leave a Reply