Best Treatment In knee Osteoarthritis

Knee Osteoarthritis (OA) is one of the most common degenerative joint diseases affecting millions of people worldwide. It is a chronic, progressive condition in which the natural cushioning between the knee bones—called articular cartilage—gradually wears away. As this protective cartilage breaks down, the bones of the knee joint begin to rub against each other, causing pain, stiffness, swelling, and difficulty in performing daily activities like walking, climbing stairs, or sitting for long periods. Although osteoarthritis can occur in any joint, the knee joint is especially prone because it bears the body’s weight and experiences continuous mechanical stress throughout life.
Knee OA is a result of a complex interaction between mechanical, biological, genetic, metabolic, and age-related factors. It is not only a disease of “wear and tear,” but also involves low-grade inflammation, changes in bone structure, and deterioration of all joint tissues, including cartilage, ligaments, synovium, and surrounding muscles. The condition typically advances slowly over years, but early recognition and treatment can significantly reduce symptoms and prevent disability.
Anatomy of the Knee Joint
To understand knee osteoarthritis, it is important to first understand the structure of the knee joint.
The knee is a large hinge joint formed by three bones:
- Femur (thigh bone)
- Tibia (shin bone)
- Patella (kneecap)
At the ends of these bones lies a smooth, slippery tissue called articular cartilage, which allows the bones to glide without friction and acts as a shock absorber. The joint is further supported by:
- Menisci (medial and lateral) that distribute weight and reduce stress
- Ligaments (ACL, PCL, MCL, LCL) providing stability
- Synovial membrane that produces fluid for lubrication
- Muscles, mainly quadriceps and hamstrings, which provide movement and joint protection
In knee OA, these structures are progressively damaged. Cartilage thins out, bone surfaces become rough, the synovial lining inflames, and small bony outgrowths known as osteophytes form.
Causes and Risk Factors
Knee Osteoarthritis has no single cause; instead, it results from a combination of factors:
1. Age
The strongest risk factor. As people age, cartilage loses its elasticity and shock-absorbing ability.
2. Obesity
Excess body weight increases joint stress. Every extra kilogram of body weight adds up to 4–6 kg of force on the knee joint during activities like climbing stairs. Obesity also releases inflammatory chemicals that accelerate cartilage breakdown.
3. Previous Knee Injury
Trauma due to accidents, ligament tears, fractures, or meniscus injury can cause early OA even in young adults.
4. Genetics
Family history plays a significant role. Certain genes can predispose a person to early cartilage breakdown.
5. Occupation
Jobs involving repetitive squatting, kneeling, lifting heavy loads, or standing for long hours increase stress on the knee.
6. Gender
Women—especially after menopause—are more likely to develop OA due to hormonal changes affecting cartilage metabolism.
7. Muscle Weakness
Weak quadriceps increase load on knee cartilage and reduce joint stability.
8. Poor Alignment
Knee deformities like bow-legs (varus) or knock-knees (valgus) cause uneven distribution of forces, accelerating cartilage wear.
9. Sedentary Lifestyle
Lack of movement reduces joint lubrication and weakens supporting muscles.
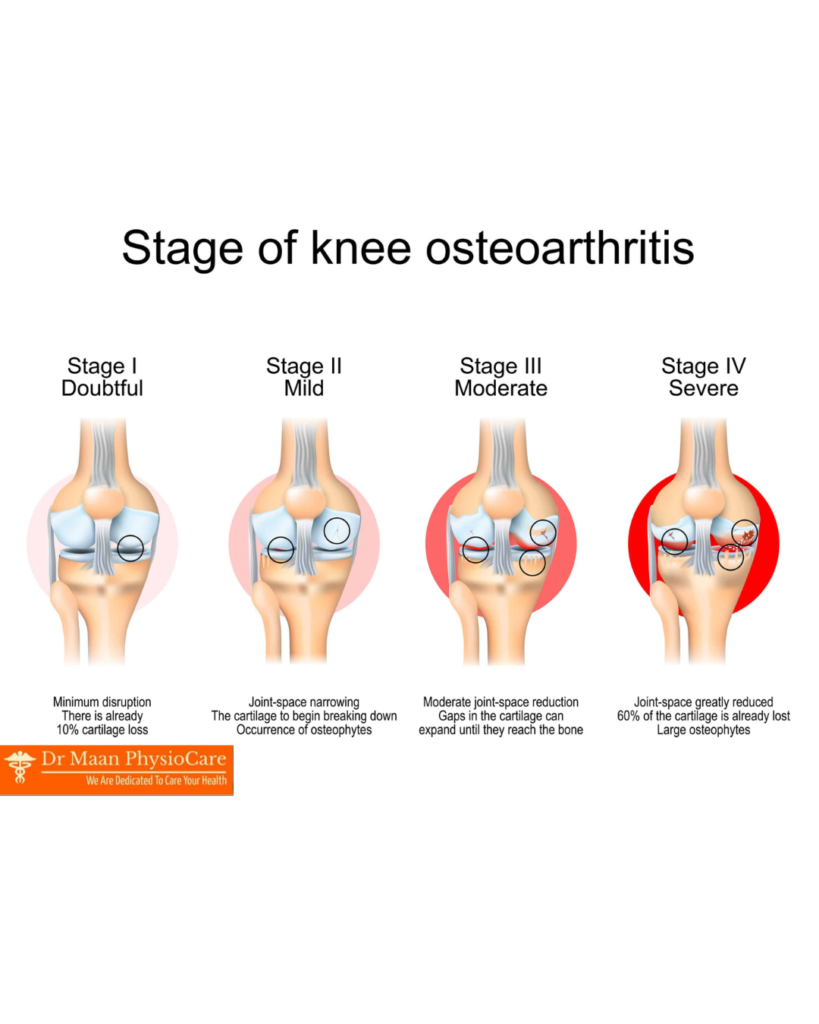
🔵 Stage 1 – Early / Doubtful OA
Features:
- Very mild cartilage wear
- Tiny bone spurs (osteophytes) may appear
- Joint space is normal
- Pain is occasional or very mild
- Stiffness lasts only a few minutes in the morning
Symptoms:
– Slight discomfort after long activity
– No major change in walking or daily activities
Diagnosis:
– X-ray may show very small osteophytes
🟡 Stage 2 – Mild OA
Features:
- Clear osteophyte formation
- Joint space begins to narrow
- Cartilage starts thinning
Symptoms:
– Pain during walking, running, climbing stairs
– Early morning stiffness
– Slight swelling after activity
– Mild crepitus (crackling sound)
Functional status:
– Daily activities are possible but painful
– Most patients start seeking medical help
🟠 Stage 3 – Moderate OA
Features:
- Moderate cartilage loss
- Joint space significantly narrowed
- More osteophytes and bone thickening
- Synovial inflammation may increase
Symptoms:
– Frequent pain even during routine walking
– Visible swelling of the knee
– Increased stiffness, especially after sitting for long
– Clear crepitus
– Occasional locking or giving-way feeling
Functional status:
– Difficult to sit cross-legged or squat
– Trouble climbing stairs
– Pain interferes with sleep sometimes
🔴 Stage 4 – Severe / End-Stage OA
Features:
- Almost complete loss of cartilage
- Bones rub directly on each other
- Very narrow or no joint space visible
- Large osteophytes
- Knee deformity (bow-legs or knock-knees)
Symptoms:
– Severe pain even at rest
– Constant stiffness
– Significant swelling and inflammation
– Difficulty walking or standing
– High risk of falling due to instability
Functional status:
– Daily activities become severely limited
– Quality of life significantly affected
Treatment at this stage:
– Usually requires Total Knee Replacement (TKR) if physiotherapy and injections fail


Leave a Reply